Lymphoid Tissue
All lymphoid cells originate from the same lymphoid progenitor cell. These can form B cells, plasma cells (differentiated B cells), T cells, and Natural Killer T cells.
Organization of Lymphoid Tissue
Central lymphoid Organs
Location of lymphocytic development.
Bone marrow: Lymphoid stem cells producing B-cells
Thymus: Accepts stem cells from bone marrow to mature T-cells
Peripheral lymphoid organs
Responsible for antigen surveillance. Are either encapsulated (E) by tissue or unencapsulated (U).
(E) Lymph nodes: Filter lymph fluid
(E) Spleen: Filters blood, removes old Red Blood Cells/Sickle Cells
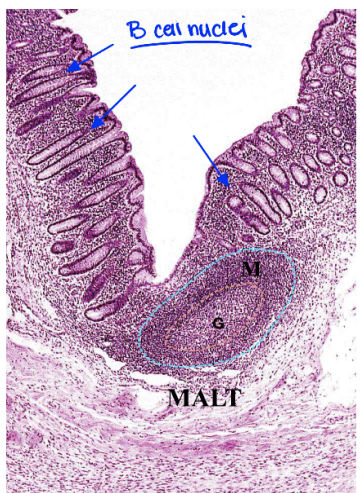
(U) Mucosa-Associated Lymphoid Tissue (MALT): Antigen surveillance along mucosal surfaces. Accounts for 85% of all lymphoid tissue.
Lymphocyte Ecotaxis
Lymphocyte migration from thymus and bone marrow to lymphoid organs. Facilitated by chemokines produced by lymphoid tissues.
High endothelial venules (HEVs) allow circulating lymphocytes to enter the organ by squeezing through spaces between cuboidal epithelial cells. These cuboidal cells contain surface receptors for integrins called vascular addressins which recruit lymphocytes to different peripheral organs. Lymphocytes will follow these integrin-addressin interactions.
The distribution of B and T cells is not uniform across the body. Blood/lymphatic fluid has more T cells than B cells whereas mucosal tissue has more B cells than T cells.
Location and Function
Circulating lymphocytes
Found in blood and lymph. Composed of 75% T cells, 10% B cells, and 15% Natural Killer T cells.
Function: Travel through blood to reach target immune sites when activated.
Features: Large, dark-staining, spherical nucleus
Diffuse lymphoid tissue
Found in mucus membranes like the respiratory tract, GI tract, urogenital tracts, and some glands.
Function: Secretes Immunoglobulin A (IgA) which protects mucosa from pathogens.
Features: Lamina propria contain a lot of B cells, eosinophils, and plasma cells
Immunoglobulin A mechanism
- Plasma cells release IgA as dimers
- IgA enters endothelial cells of mucosa
- IgA binds a secretory component, protecting it from degradation from lysosomes
- Secretory component with IgA is released
Solitary Nodules
Encapsulated aggregations of lymphocytes (MALTs) found in mucus membranes like the respiratory tract, GI tract, urogenital tracts, and some glands. Contains a primary follicle of unactivated B cells and a secondary follicle which has a cap of unactivated B cells plus a germinal center where the cells are activated (will also contain Helper T cells, dendritic cells, etc.).
Function: Forms when B cells aggregate at site of infection.
Features: Cap stains dark (denser), germinal center stains light
Aggregated nodules
Solid nodules within a tissue or organ.
Tonsils
Found in pharyngeal opening, oral cavity, and base of tongue.
Function: First line defense against incoming pathogens
Features: Incompletely encapsulated, the luminal surface is covered with stratified squamous non-keratinized epithelium. Also has crypts or pleats.
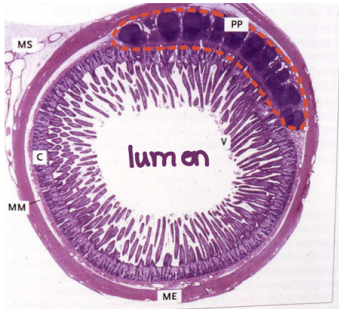
Peyer's Patches
Found in lamina propria of the small intestine (especially the ileum).
Function: Monitors mucous membranes for pathogens, initiates secretory immune response with M cells which present the pathogens to macrophages
Features: Visible with naked eye
Vermiform Appendix
Found in terminal tip of cecum (large intestine).
Function: Not well understood.
Features: Has a lot of lymphatic nodules.
Clinical Pearl: McBurney's Point
Located in Right Lower Quadrant. Tenderness at this point is a sign of acute appendicitis.
Lymphoid Organs
Bone Marrow
Found in center of most bones.
For more see: Hematopoeisis
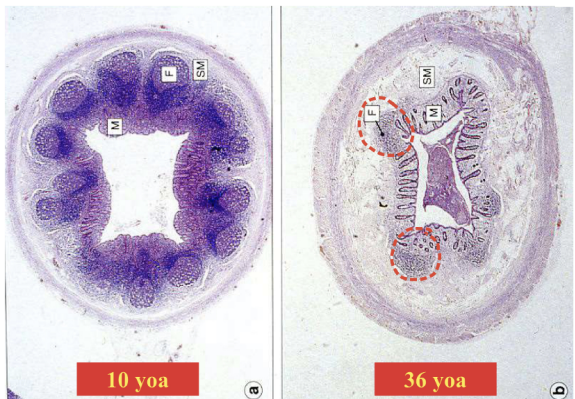
Thymus
Found in superior mediastinum. Epithelial reticular cells provide the framework for T cell maturation. The cortex prevents developing thymocytes from contacting the capillaries which could cause an immune response. The medulla contains Hassall's corpuscles, composed of aggregated epithelial reticular cells which secrete cytokines.
With age, the density of lymphoid tissue/T cell production decreases leaving mostly adipose tissue.
Function: T cell maturation site (immunoselection, 95% of thymocytes are not selected and destroyed)
Features: Connective capsule, trabeculae divides thymus into lobules. The cortex is dark while the medulla is light.
Lymph nodes
Found all over the body (>500 locations), but especially the neck, axillae, mediastinum, and retroperitoneum. The superficial cortex contains type 1/2 nodules (B cells) while the deep cortex contains T cells. The medulla contains plasma cells.
Function: Filters lymph, stores B and T cells
Features: Contains afferent and efferent lymphatic vessels. Reticular cells form a framework of nodes rich in Type III collagen
Spleen
Found in left upper quadrant of abdomen. Circulation can be open and slow or closed and fast.
Function: Filters blood using sinusoids (leaky capillary) which does not allow damaged red blood cells to re-enter circulation because of their rigidity. Will also store platelets, respond to blood-borne antigens and perform hematopoiesis in the fetus.
Features: White pulp is rich in lymphocytes. Specifically, the periarterial lymphatic sheath (PALS) is T cell rich whereas the follicles are B cell rich. Additionally, the red pulp contains sinusoids and is rich in erythrocytes