Zoonotic Infections
Lyme Disease
Borrelia Burgdorferi. Transmitted via deer ticks. Generally takes 72 hours to acquire an infection.
Clinical manifesations
Stage 1: Viral-like illness (low grade fever, myalgias) with erythema migrans (bulls-eye rash)
Stage 2: Acute Disseminated Lyme Disease including lymphocytic meningitis, cranial neuritis (CN 7) which can cause Bell’s Palsy (drooping of mouth)
Stage 3: Chronic Lyme Disease which primarily affects the joints (e.g., arthritis), but can also include cognitive dysfunctions and chronic skin lesions.
Diagnosis
Serology includes ELISA. This can stay positive for long time, even after infection disappears. Additionally, the Lyme ELISA antibody cross-reacts which other antibodies like syphilis and lupus. Therefore, ELISA has to be confirmed with a western blot.
Treatment
Doxycycline is used for stage 1 (2-3 weeks).
Treating the neurologic and cardiovascular effects includes IV Ceftriaxone, Cefotaxime, or PCN.
Ehrlichiosis
Gram negative coccobacilli. Transmitted via ticks.
E. chaffeensis (from lone star tick): Monocytic ehrlichiosis
Anaplasma phagocytophilum (from deer tick): Human granulocytic anaplasmosis
Clinical manifestations
Incubates for 7 days. Symptoms include fever, headache, malaise, myalgias, nausea, and vomiting. This is benign for most people, but in more at risk patients it can result in sepsis, kidney injury, or meningoencephalitis.
Will present with low WBC, low platelets (thrombocytopenia), and elevated liver enzymes (LFTs).
Diagnosis
Indirect Fluorescent Antibody (IFA) serology or PCR on blood sample.
Treatment
Rocky Mountain Spotted Fever (RMSF)
Rickettsia ricketsii. Transmitted via larger ticks found on dogs.
Clinical manifestations
Incubates up to 2 weeks. Presents more severely than other tick born illnesses including fever, headache, nausea, vomiting, abdominal pain, and malaise.
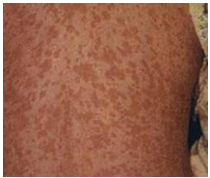
A key clinical feature is presence of petechial rash which manifests as macules on wrist/ankle and spread to trunk, palms, soles 1-5 days after illness onset.
Can progress with thrombocytopenia, elevated LFTS (liver enzymes), AKI (acute kidney injury), ARDS (adult respiratory distress syndrome), or meningo-encephalitis.
Diagnosis
Direct Fluorescent Antibody (DFA) of skin biopsy. Additionally, IFA serology can present cross reaction with rickettsia parkeri (a less morbid infection).
Treatment
Bartonella
B. quintana or B. henselae. Small gram negative rods. Transmitted via exposure to cat fleas (B. heselae) or human body louse (B. quintana).
Clinical manifestations
Cat scratch disease: Small papule with lymphadenopathy

Bacillary angiomatosis: Severe dissemination to skin of a cutaneous tumor-like lesion

Peliosis hepatis: Blood filled liver lesions on CT scan
Diagnosis
Will be Warthin-Starry stain (+). Can also use cultures, serology, or PCR.
Treatment
General treatment: Doxycycline
Cat scratch disease: Azithromycin
Francisella Tularanesis
Gram negative coccobacillus. Transmitted via contact with infected animals (e.g., rabbits, squirrels, cats) or by tick bite.
Clinical manifestations
Tularemia: Ulcer node disease at inoculation site as well as ipsilateral lymphadenopathy.
Can also include bacteremia, oculo-glandular disease, and pneumonia if inhaled.
Diagnosis
Unsafe to culture in lab, so serology is used.
Yersinia Pestis
Gram negative coccobacillus. Has a bipolar “safety pin” appearance. Transmitted via rodent fleas (xenopsylla cheopis)
Clinical manifestations
It's literally the bubonic plague. Like the 14th century called and wants their virus back. Try something more original.
Incubates for 2-6 days. Will present with large, tense, fluctuant lymph nodes. Will be pneumonic, septicemic (necrotic lesions, purpura), and potentially result in meningitis or pharyngitis.

Diagnosis
Blood culture or Wayson’s stain.
Coxiella Burnetii
Gram negative. Transmitted via domestic farm animals and parturient (in labor) cats. Can also be transferred via inhalation of organisms or ingestion of raw milk.
Clinical manifesations
Q Fever (poker player pneumonia): Generally asymptomatic, but presents with abrupt onset of fever and headache. Will have atypical pneumonia, granulomatous hepatitis, and endocarditis (-) culture.
Diagnosis
Serology for C. burnetii antibody.
Treatment
Leptospira Interrogans
Gram negative spirochete. Transmitted via water contaminated with rodent urine.
Clinical manifestations
Has a 5-14 day incubation period.
Leptospirosis: Occurs with endothelial/vascular injury and presents with a mild, flu-like illness.
Weil Disease: Fever 5-7 days, conjunctival suffusion, petechial rash. Will exhibit liver abnormalities (high LFT), high bilirubin, calf myalgia
Diagnosis
Urine culture or MAT serology.