Antibiotics
Lab Standards
Minimal Inhibitory Concentration (MIC) is the minimal concentration of antibiotic that prevents the clear suspension CFU from becoming turbid after overnight inoculation. Essentially, the lowest level of antimicrobial agent resulting in microbial death.
The Microbroth Dilution Method is the gold standard for determining MIC. The three descriptive categories are S (sensitive), I (intermediate), and R (resistant).
For each bacterium and antibiotic combo, there will be a different specific MIC, known as the MIC break point. An Antibiogram tracks the resistance of different strains of bacteria in a specific location.
Distribution
Knowing the distribution properties of a drug can help us choose a specific drug based on the site of the infection. A high distribution to a tissue compartment is often correlated with a low distribution in the blood or urine.
Pediatric patients have a higher proportion of water content, so hydrophilic agents will distribute well in younger patients and lipophilic agents will not. In obese patients, lipophilic agents may get trapped in adipose tissue.
Hydrophilic antibiotics: Beta Lactams, Aminoglycosides, Vancomycin
Lipophilic antibiotics: Quinolones, Oxazolidinones, SMX-TMP, Tetracyclines, Metronidazole
Blood brain barrier
Many drugs cannot cross the BBB unless they are lipophilic and can diffuse across the membrane. Drugs with flow-limited distribution (lipophilic) are preferred.
Permeable drugs
- 3rd & 4th generation Cephalosporins
- Carbapenems
- SMX-TMP
- Quinolones
- Oxazolidinones
- Metronidazole
Non-permeable drugs
- Aminoglycosides
- Vancomycin
- Clindamycin
- Macrolides
Elimination
Hepatic metabolism
It is difficult to quantify hepatic function; dose adjust for mod-severe impairment
Examples
- Macrolides
- Tetracyclines
- Clindamycin
Renal metabolism
It is much easier to quantify renal function using CrCl and urine output. Assume that these drugs are removed by hemodialysis and require redosing after hemodialysis. For someone with impaired renal function, a much lower dose of antibiotics is required over a longer period of time.
Examples
- Beta-Lactams
- Quinolones
- Vancomycin
- Aminoglycosides
Pharmacodynamics
Time-dependent microbials
Duration of antimicrobial exposure is most important for these drugs and optimal bactericidal activity occurs when serum drug level reaches a dosing threshold (usually 4-5x the MIC). Higher drug levels do not increase the rate or extent of bacterial killing.
Examples
- Beta-lactams: Penicillins, Cephalosporins, Carbapenems
Concentration-dependent microbials
Concentration of drug is most important with these drugs for bacteriologic eradication and the higher the drug concentration, the greater the rate and extent of bacterial killing.
Examples
- Aminoglycosides
- Fluoroquinolones
- Vancomycin
Dosing Nomograms
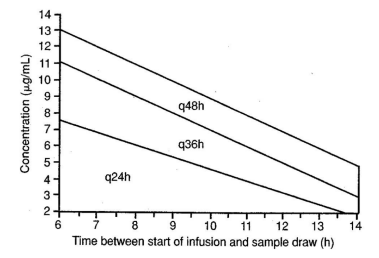
Find the point of intersection between the delivered dosage and the time since infusion. This point corresponds with the time of dose.
In the example below, an checking serum concentration 10 hours after an initial dose of 7mg/kg would correspond with the interval q36h, or a subsequent dose recommended in 36 hours.
Beta-lactams
Beta-lactam agents inhibit cell wall synthesis via formation of covalent bond with PBP to prevent further formation of peptidoglycan. These include Penicillins, Cephalosporins, Carbapenems, and Monobactams.
Glycopeptides, like Vancomycin, bind to D-alanine.
Penicillins (PCNs)
Beta-Lactam. Narrow spectrum and most do not cover S. aureus. The exception to this is Nafcillin.
Indications
- Oral pharyngeal infections: [[Gram Positive Cocci#Group A Streptococcus pyogenes|Group A Strep]] pharyngitis, dental abscess
- Skin & Soft Tissue Infections: Group A Strep necrotizing fasciitis, Group A Strep impetigo
- Endocarditis
- Meningitis
- Syphilis (Treponema pallidum)
Amino-Penicillins
Beta-Lactam. Includes amoxicillin (oral) and ampicillin (IV/oral). Spectrum of activity is narrow and similar to PCN. No longer active against Gram (-) bacilli due to beta-lactamase production.
Indications
- Endocarditis (Enterococcus)
- UTI (Enterococcus)
- Intra-abdominal abscess (Enterococcus)
- Meningitis (Listeria monocytogenes)
- Immunocompromised patients (Listeria monocytogenes)
Amino-PCNs + Beta-Lactamase Inhibitor (BLI)
The beta-lactamase inhibitor protects the beta-lactam agent from enzymatic degradation.
Amoxicillin + Clavulanate (PO) (Augmentin)
Indicated for otitis, sinusitis, bronchitis, and bite wounds
- Active against S. aureus
- Active against aerobic/anaerobic gram negative rods
- Active aerobic bacteria: E. coli, Klebsiella, H. influenzae, Proteus
- Active anaerobic bacteria: Bacteroides
Ampicillin + Sulbactam (IV) (Unasyn)
Indicated for intra-abdominal, gynecological infection
- Same activity as Amoxicillin + Clavulanate, but also has activity towards Acinetobacter
Extended Spectrum PCNs (anti-pseudomonal)
Beta-lactamase inhibitor extends activity against aerobic and anaerobic gram negative rods, including P. aeruginosa and S. aureus.
Piperacillin + Tazobactam (Zosyn)
Indicated for Hospital Acquired Infections, HAP/VAP, UTI, intra-abdominal infection, diabetic limb infection, and severe Pseudomonas infection
Cephalosporins
Beta-Lactam. Note: No cephalosporin covers enterococci.
| Generation | Indication | Notes | |
|---|---|---|---|
| Cefazolin | 1 | MSSA and surgical prophylaxis | Great gram positive coverage |
| Cefuroxime | 2 | Sinusitis, bronchitis, and otitis | |
| Cefotetan/cefoxitin | 2 | Only ceph with anaerobic coverage | |
| Ceftriaxone | 3 | Community acquired pneumonia/meningitis | Eliminated via biliary clearance, contraindicated for biliary diseases |
| Ceftazidime | 3 | Pseudomonas | |
| Cefepime | 4 | Hospital acquired pneumonia/meningitis and other infections | GPC and GNR coverage |
| Ceftaroline | 5 | MRSA, SSTI, community acquired pneumonia | |
| 3rd and 4th generation cephalosporins can penetrate the blood brain barrier |
Advanced Generation Cephalosporins
Ceftolozane + Tazobactam
Advanced generation ceph + beta-lactamase inhibitor.
Treatment for multidrug resistant pseudomonas
Ceftazidime + Avibactam
3rd generation ceph + beta-lactamase inhibitor.
Treatment for multidrug resistant hospital acquired infections and carbapenem resistant enterobacterials (CRE)
Cefiderocol
Advanced generation ceph.
Last line of defense against multidrug resistant hospital acquired gram negative rods.
Carbapenems
Resists degradation against most Beta-lactamase enzymes.
Meropenem + Vaborbactam
Treatment for multidrug resistant hospital acquired infections and carbapenem resistant enterobacterials (CRE).
Aztreonam
A monobactam.
Treatment for pseudomonas and it is used for patients with severe B-lactam allergy.
Imipenem + Cilastatin
Cilastatin prevents Imipenem from being degraded by kidney enzyme dehydropeptidase. Carries some seizure risk.
Treatment for multidrug resistant hospital acquired infections, pseudomonas, and extended-spectrum beta-lactamases.
Meropenem
Lower risk of seizure than Imipenem + Cilastatin.
Treatment for multidrug resistant hospital acquired infections, pseudomonas, and extended-spectrum beta-lactamases.
Ertapenem
Covers extended-spectrum beta-lactamases, but not pseudomonas.
Agents for Resistant Gram Positive Cocci
Vancomycin
Poor oral absorption, 30-50% bound to plasma protein, low volume of distribution. Covers multidrug resistant S. aureus (MRSA).
Daptomycin
Covers multidrug resistant S. aureus (MRSA) and vancomycin-resistant enterococci.
Protein Synthesis Inhibitors
Self-explanatory.
Classes
- Glycylcyclines
- Macrolides
- Aminoglycosides
- Lincosamides
- Oxazolidinones
- Tetracyclines
All of these classes inhibit the 50s subunit of the ribosome, except for the Aminoglycosides and Tetracyclines, which inhibit 30s.
Note: Aminoglycosides have a persistent effect even with undetectable serum levels.
Oxazolidinones
Linezolid
A weak MAO inhibitor, so watch out for other serotonergic drugs.
Covers multidrug resistant S. aureus (MRSA).
Lincosamides
Clindamycin
Inhibits toxin formation.
Used for anaerobes above the diaphragm (which tend to be more gram positive).
Aminoglycosides
Gentamicin, tobramycin, amikacin
Bad for your kidneys.
Covers resistant gram negative rods.
Macrolides
These drugs are great for atypical bacteria like chlamydia, mycoplasma, and legionella.
Azithromycin (Z-pack)
Not metabolized by CYP3A4 in the liver and has a very long half life
Used for community acquired sinusitis, bronchitis, and otitis.
Fidaxomicin
Spares the microbiome which is nice.
Treats C. diff colitis, but vancomycin is the drug of choice for that.
Tetracyclines
Doxycycline
First-line treatment for tick-borne illnesses.
Metabolic Pathway Disrupter
Sulfamethoxazole + Trimethoprim (SMX-TMP)
Inhibits Dihydrofolate Reductase, needed to make bacterial folate
Indications
- Stenotrophomonas
- Gram positive cocci (like MRSA)
- Gram negative rods
- Pneumocystis (fungal infection)
- E. coli
- UTI
Glycylcyclines
Ervacycline
Treatment for resistant gram positive cocci, extended-spectrum beta-lactamases and other multidrug resistant organisms.
Nucleic Acid Synthesis Inhibitors
Classes
- Fluoroquinolones
- Metronidazole
- Rifamycin (not covered here)
Fluoroquinolones
Inhibit DNA gyrase (topoisomerase II and IV)
Ciprofloxacin, levofloxacin, moxifloxacin
Cover gram negative rods and atypical pathogens like chlamydia, mycoplasma, and legionella. The exception is that moxifloxacin does not cover pseudomonas. Also good for treating community acquired infections.
??
We don't know how this works.
Metronidazole
Used for anaerobes below the diaphragm (which tend to be more gram negative).