Adrenergics
The sympathetic nervous system emerges from the thoracic-lumbar region of the spine. It will synapse with sympathetic chain ganglia and release norepinephrine on targets.
Pre-ganglionic neurons synapse with the Adrenal Medulla which releases epinephrine and norepinephrine into the blood
Post-ganglionic neurons release dopamine for renal smooth muscle.
Receptors
See here for a primer on signaling subunits s, i, and q: Signal Transduction Primer > Guanine binding proteins
Alpha 1 (Sympathetic)
Found in blood vessel smooth muscle, eyes, gastrointestinal system, and prostate. Dilates eyes, decreases gastrointestinal motility, contracts prostate (A1A), through vasoconstriction.
Alpha 1 receptors are innervated via sympathetic tone which increases total peripheral resistance (and diastolic blood pressure), as well as venous tone (and systolic blood pressure).
Muscle contraction mechanism
Gq → phospholipase C → Ca2+ → contraction
Clinical pearl: Benign prostatic hyperplasia
Blocking Alpha 1 activation can relax the prostate, which makes it easier for patients with BPH to urinate. The drug in question is Tamsulosin.
Alpha 2A (Parasympathetic)
These are inhibitory receptors. They are found in the vasomotor center of the medulla (CNS) and pre-synaptic terminals.
In the CNS, A2A inhibits Sympathetic Cardiovascular Outflow (generally decreasing all things heart).
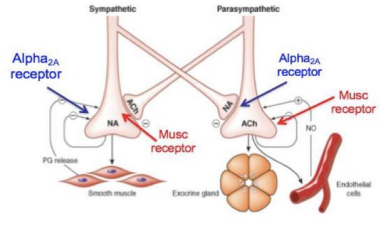
In pre-synaptic terminals, A2A downregulates norepinephrine/acetylcholine, preventing stimulation of the SNS/PNS. Norepinephrine released from nerve terminals come back to bind at an A2A receptor, regulating the output.
A2A is important for reciprocal inhibition between the sympathetic and parasympathetic systems. For example, when the sympathetic system is upregulated, it will cross signal to an A2A receptor in the parasympathetic system to downregulate it and vice versa.
Alpha 2B (Sympathetic)
Found in blood vessels. These vasoconstrict (increasing total peripheral resistance).
Muscle contraction mechanism
Gi → decrease adenylyl cyclase → decrease cAMP → contraction
Beta 1 (Sympathetic)
Found in the heart and kidneys. Increases all things heart as well as renin in the kidneys and blood volume.
Muscle contraction mechanism
Gs → increase adenylyl cyclase → increase cAMP → relaxation
Beta 2 (Sympathetic)
Has much higher affinity for epinephrine than norepinephrine. Found in the heart, lungs, liver, and blood vessels in skeletal muscle/liver. It will increase heart rate, bronchodilate, and dilate vessels in the skeletal muscles and liver.
Muscle contraction mechanism
Gs → increase adenylyl cyclase → increase cAMP → relaxation
Beta 3 (Sympathetic)
Found in bladder and fat cells. Decreases bladder smooth muscle contraction (increasing urine retention) as well as decreasing lipolysis and release of free fatty acids).
Muscle contraction mechanism
Gs → increase adenylyl cyclase → increase cAMP → relaxation
Dopamine 1
Found in renal vasculature and smooth muscle. Relaxes renal vasculature and smooth muscle.
Muscle contraction mechanism
Gs → increase adenylyl cyclase → increase cAMP → relaxation
Catecholamine Metabolism
See here for the catecholamine synthesis enzymes: Synaptic Cell Biology > Key Neurotransmitter Metabolism
TL;DR
- Tyrosine → DOPA (via tyrosine hydroxylase) →→ neurotransmitter
- Tyrosine hydroxylase is the rate limiting step and requires the cofactor BH4
- Dopamine → Norepinephrine occurs inside the vesicle
- VMAT1/2 transport norepinephrine into the cell
- Norepinephrine is degraded by COMT/MAO
The production of catecholamines can be upregulated by phosphorylation of TH, which increases affinity for BH4. It can also be upregulated by transcription factors.
Clinical pearl: Reducing catecholamine levels
Tyrosine hydroxylase is the rate limiting step for catecholamine formation, which is useful to inhibit when there is overactive production of catecholamines like in the case of an Adrenal Medulla tumor. Metyrosine will do just that.
Catecholamines are transported into vesicles by VMAT, which can be targeted pharmacologically. This will decrease catecholamine levels as they will be degraded by an MAO if not protected in a vesicle.
Clinical pearl: Increasing norepinephrine effect
The transporter for norepinephrine is NET. This can be inhibited by drugs like cocaine and some anti-depressants. Blocking NET produces a prolonged effect in the synapse.
When catecholamines arrive back into the cell, they are degraded by MAO (in neurons) or COMT (in effector cells). MAO inhibitors will also increase the effect of catecholamines.
Finally, blocking A2A receptors will stop the negative feedback on norepinephrine release.
Clinical pearl: L-DOPA
L-DOPA is used instead of dopamine for the treatment of Parkinson's because it can cross the blood brain barrier while dopamine cannot.
Blood Pressure
Take a gander at this for an autonomic nervous system blood pressure review: Autonomic Nervous System Effects Primer > Heart Circulation.
Cardiac muscle
Increase in cAMP → Contraction (B1 - Heart)
Decrease in cAMP → Relaxation (M2 - Heart)
Smooth muscle
Increase in cAMP → Relaxation (B2 - e.g. Bronchi)
Decrease in cAMP → Contraction (A1 - e.g. Vasculature)
Baroreceptor Reflex
Allows the body to quickly maintain blood pressure so that we don't need to mess around with hormones and receptors.
There are stretch receptors in the carotids and aortic arch. This information is relayed down the Vagus Nerve to adjust heart rate. Baroreceptor tone is the constant signal the brain receives the stretch receptors.
Spike in blood pressure → decrease heart rate → decrease cardiac output (→ systolic blood pressure)
Secondarily, A2A receptors in the vasomotor center in the brain will trigger vasodilation, decreasing total peripheral resistance (→ diastolic blood pressure) and cardiac output (→ systolic blood pressure)
Food for thought
What if an A1 agonist (phenylephrine) was given and then atropine?
The baroreceptor signal would still be sensed by the brain, but it won't be able to transmit the signal to increase heart rate as the muscarinic receptors on the Vagus Nerve will be inhibited by the atropine.
Direct Catecholamine Action
Norepinephrine
Stimulates A1, A2B, B1, and B3 receptors (not B2).
A1/A2B → increase blood pressure
B1 → increase all things heart → increase blood pressure
As blood pressure spikes, heart rate drops to compensate.
Epinephrine (Low Dose)
Stimulates all Alpha and Beta receptors. At a low dose, B2/B1 will predominate in response.
B2 → vasodilation → lower diastolic blood pressure
B1 → increased heart rate / cardiac output → higher systolic blood pressure
No baroreceptor reflex response as mean blood pressure remains the same.