Hormonal Regulation Of Metabolism
Insulin
Secreted from pancreatic beta islets. Responds to high glucose by transporting glucose into cells via GLUT-4.
GLUT-2 is insulin independent and is used in the liver/pancreas to evaluate the blood glucose level in order to maintain homeostasis by secreting insulin or glucagon. In the brain, where glucose is the primary form of energy, an insulin independent transporter is used to bring glucose into the cell (GLUT-1/3).
Preproinsulin → proinsulin → insulin
- Preproinsulin = Peptide A + Peptide B + Peptide C + signal sequence
- Proinsulin = Peptide A + Peptide B + Peptide C
- Insulin = Peptide A + Peptide B
Because Peptide C is cleaved to form insulin, its concentration in the blood can be measured to evaluate the amount of insulin present. Diabetic patients administered insulin will not have Peptide C in their blood.
Signal Transduction
Release
The pancreas uses GLUT-2 transporters, meaning the glucose levels in the blood and pancreatic beta cells will be the same. As glucose enters the cell, they are trapped via conversion to G6P by glucokinase, increasing the rate of ATP production. As ATP binds to ATP gated potassium channels, closing them, the membrane depolarizes and begins to gain Ca2+ via voltage gated calcium channels. The calcium will bind to insulin granules which release via exocytosis.
- Glucose enters and is converted to G6P → energy production (ATP)
- ATP concentration increases → Binds potassium channels
- Potassium channels close → Depolarization
- Depolarization → Ca2+ channels open
- Ca2+ binds insulin granules → insulin release
Downstream effects
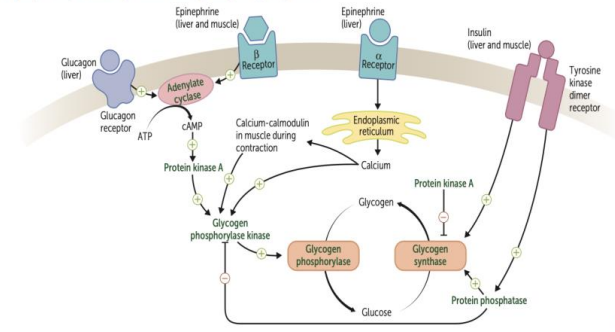
As insulin is released, it binds to the insulin receptor (a Tyrosine Kinase Receptor). This will stimulate Protein Kinase B (PKB) which increases insertion of GLUT-4 in the cell membrane (more glucose uptake). It will also phosphorylate glycogen synthase kinase (GSK) (inactivating it) so that glycogen synthase remains in its inactive, phosphorylated state.
The glucose can then be converted to glycerol-3-phosphate (G3P) from DHAP (glycolysis) for TAG formation.
Glucagon
Secreted from pancreatic alpha islets. Responds to low glucose breaking down glycogen in the liver by lowering Fructose-2,6-Bisphosphate (F26BP) concentrations, an upregulator of PFK-1 in the glycolysis.
It will also inhibit glycogen synthesis by phosphorylating glycogen synthase as well as inhibit fatty acid synthesis by inhibiting acetyl-CoA carboxylase via cAMP activation of protein kinase A (PKA). PKA has the secondary function of activating lipase in adipocytes to break down TAGs.
Signal transduction
The glucagon receptor is a GPCR receptor.
- Gs → cAMP
- cAMP → PKA
- PKA → inhibit acetyl-CoA carboxylase, activate lipase
Catecholamines (Norepinephrine/Epinephrine)
For more detail on receptor function, see here: Adrenergics
These function similarly to glucagon and will also stimulate glucagon secretion and inhibit insulin. They will promote glycogenolysis, gluconeogenesis, and fatty acid breakdown.
These hormones will also switch muscles to fatty acid usage for energy by blocking glucose uptake.
Catecholamines and exercise
With exercise, these endorphins will inhibit insulin. In order to get glucose back into the cell to maintain energy, the AMP-activated protein kinase (AMP-K) pathway is activated through the energy expenditure (ATP → AMP). This will promote insertion of GLUT-4 transporters into the cell membrane which increase glucose uptake.
This is why exercise is important for diabetic patients as it helps lower blood glucose.
Signal transduction
Catecholamines bind beta adrenergic receptors, which are GPCR receptors.
- Gs → cAMP
- cAMP→ PKA
- PKA → inhibit acetyl-CoA carboxylase, activate lipase
They will also bind alpha adrenergic receptors, which are GPCR receptors.
- Gq → PIP2
- PIP2 → IP3 and DAG (via PLC)
- DAG → PKC (via Ca2+)
PKC: C for calcium!
Leptin
Released by adipose tissue, which informs the body it is satiated. It will promote beta-oxidation and downregulate TAG synthesis. It will interact with the hypothalamus by promoting release of norepinephrine. It will also increase cellular insulin sensitivity as leptin and insulin share a signaling pathway.
Leptin will also activate AMP kinase (AMPK). In the muscle, AMPK will increase uptake of fatty acids and glucose. In the liver, AMPK will slow down fatty acid synthesis.
Adiponectin is another peptide hormone released by adipose which upregulates AMPK.