Mesoderm - Cardiovascular
Formation of Embryonic Mesoderm
Previously on mesoderm: Gastrulation and Embryonic Folding > 2a. Mesoderm and Ectoderm
Derived from epiblast cells (primitive ectoderm) which are the second batch to ingress through the primitive streak. Signaling from the endoderm will signal the ingressing cells to become the mesoderm.
Organs from the mesoderm
Mesoderm cells converge onto each other, causing them to extend. Inductive intracellular signaling will lead to the formation of the 3 mesodermal regions.
Paraxial mesoderm
Para refers to being nearest to neural tube/notochord. Forms the head and somites.
Somites
Cells surrounding the neural tube. By week 3, there will be 40 pairs of somites.
Sclerotome: Forms cartilage of the vertebra and ribs
Myotome: Forms skeletal muscle of the neck, trunk, and limbs
Dermatome: Forms dermis and skeletal muscle of the dorsal part of the body
- Syndotome: Forms tendons
- Endothelial cells
Intermediate mesoderm
Forms the urogenital system (kidney's and gonads)
Lateral plate mesoderm
Lateral refers to the farthest from the neural tube/notochord. By week 3, this subdivides into the splanchnic and somatic mesoderm.
Splanchnic: Forms the circulatory system
Somatic: Forms body cavities and pelvis
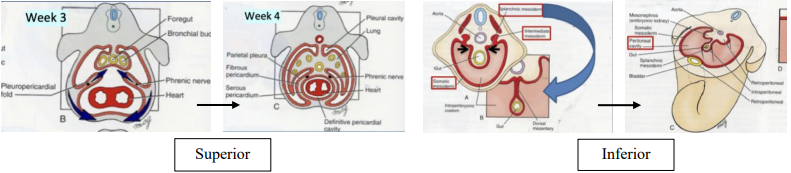
New body cavities
The somatic mesoderm grows over the splanchnic mesoderm, creating the intraembryonic cavity. This is the source of all body cavities. Overgrowth of the somatic mesoderm will cause the splanchnic mesoderm to fuse, forming the dorsal mesentery which holds the gut tube in place.
Pericardial cavity: Surrounds the heart
Peritoneal cavity: Abdominal organ space
Pleural cavity: Surrounds the lungs
Heart tube formation
This is the first functional organ to form.
Day 15: Mesoderm cells spread cranially, giving rise to the primary heart field. Some beating, no blood movement.
Day 21: Two ends of the primary heart field fuse to form a heart tube which starts pumping blood.
Day 22-24: D-looping allows the vessels of the heart to migrate to destinations. The atria are initially inferior to the ventricles and must loop cranially to reach the final location.
Day 28: The aortic sac region will give rise to the aortic arches. The atrioventricular valve (AVV) cushion is present, but only joined with the left ventricle.
Day 50: Heart formation is completed and will grow in size.
Hemodynamic load
The major driving force for cardiomyocyte proliferation. Increase in red blood cells creates an increase in pressure against heart walls, stimulating cell proliferation. Hypertrophy of cardiomyocytes also contributes to growth.
Neuregulin: Induces cardiomyocytes to continue growing. Can be used in cardiac therapy to regrow infarcted regions of the heart post-heart attack.
Cardiac valves: Derived from from cardiac cushions which are regional swellings of ECM.
Blood formation
Blood vessels arise either from vasculogenisis or angiogenesis.
Vasculogenesis
Formation of blood vessels from non-blood vessels. First occurs in the secondary yolk sac. Mesoderm cells in the embryo have a hard time getting oxygen, and those in the center produce vascular endothelial growth factor (VEGF). VEGF binds to receptors FLK-1 or FLK-2 which signals the mesoderm cells to become hemangioblasts. These will produce endothelial cells (lining of blood vessels) and blood cells (blood islets).
For more VEGF, see also: Fertilization and Implantation > Pre-eclampsia
Angiogenesis
Formation of blood vessels from existing blood vessels. Starts in the secondary yolk sac. By day 23, definitive hematopoietic stem cells (dHSCs) will form in the lover for utero blood formation. Blood formation in long bones does not take place until week 10.
Clinical pearls
Acyanotic heart defects
Left/right mixing of blood
Ventricular septal defect: the separation between the ventricles does not fully form
Patent ductus arteriosus: the ductus arteriosus remains open
Atrial septal defect: a hole is present between the two atria
Outflow obstruction
Pulmonary stenosis: The opening of the pulmonary valve is narrowed
Aortic stenosis: The opening of the aortic valve is narrowed
Coarctation of the aorta: Narrowing of a part of the aorta
Cyanotic heart defects
Tetralogy of Fallot
Narrowed pulmonary trunk, pulmonary stenosis, ventricular septal defect, and a thickened right ventricular wall
Transposition of the great arteries
The aorta connects to the right ventricle and the pulmonary artery connects to the left ventricle
Atrioventricular septal defect – complete
A hole at the center of the heart where the walls of the atria and ventricles meet and only one valve separates the atria and ventricles
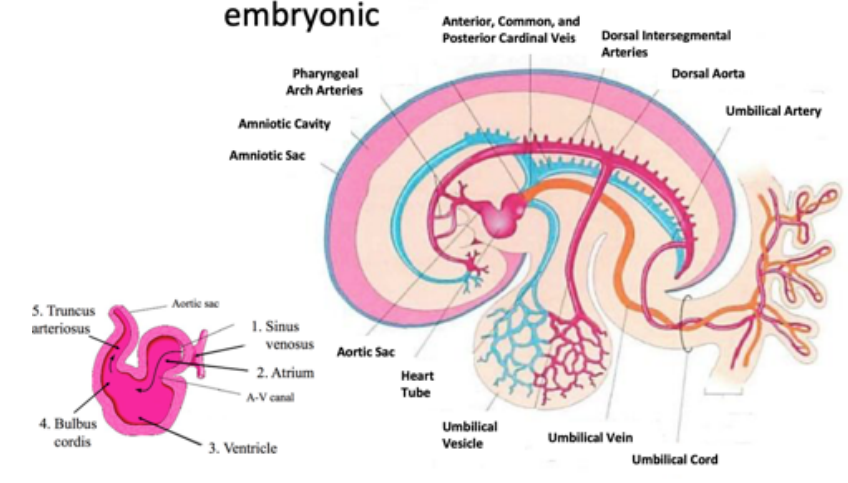
Embryonic Circulatory System
- Blood (oxygenated) flows from the placenta to the umbilical vein
- Blood enters the heart tube at the sinus venosus
- Blood enters the atrium, mixing with deoxygenated blood from the common cardinal vein
- AV-canal → Ventricle → Bulbus Cordis → Truncus Arteriosus
- Blood flows through the pharyngeal/aortic arches and into the internal carotid artery towards the head/dorsal aorta
- Blood diverts into the vitelline vessels/intersegmental vessels/iliac vessels
- Blood returns to the heart via cardinal veins and the vitelline vein
When blood returns to the heart, much of it is shunted from the aorta to the umbilical artery (oxygenated in the placenta)
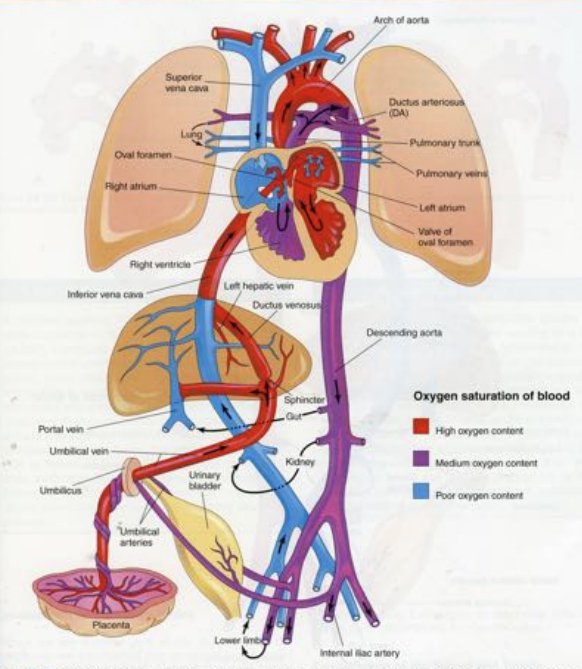
Fetal blood flow
- Blood arrives from the placenta via the umbilical vein
- Blood is shunted away from liver (as it is not yet fully functioning) through the ductus venosis into the right atrium/inferior vena cava
- Blood flows into left atrium through the foramen ovale (opening between atria)
- Blood flows from left atrium to the left ventricle to the aorta
- Blood is also shunted from the lungs through the ductus arteriosus which connects to the pulmonary artery
- Blood flows to the head and body
- Deoxygenated blood returns to the placenta through the umbilical arteries (2 umbilical arteries, 1 umbilical vein)
Blood flows into the right atrium of the heart via the ductus venosus (DV) and the IVC. Therefore, blood flowing into the RV is mixed. The blood flowing from the right atrium to the left atrium flows via the foramen ovale.
Some of the blood from the DV/IVC flows into the RV via the tricuspid valve. Most of the blood from the SVC flows into the RA and then to the RV via the tricuspid valve.
Circulatory System Changes Post-Birth
Ductus arteriosus constricts, forming the ligamentum arteriosum.
Umbilical vessels constrict and degrade.
Foramen ovale closes, forming the fossa ovalis.
Clinical pearl: Patent Ductus Arteriosus
When the ductus arteriosus does not close and forms the ligamentum arteriosum after birth. This causes oxygenated blood to be diverted from the aorta to the pulmonary circulation via the pulmonary arteries. A large PDA will put strain on the lungs and could require intervention.
This is an acyanotic left to right shunt.
Arterial System
Aortic arch arteries
Blood flows out of truncus arteriosus (becomes the aortic sac around day 24) and into the pharyngeal arch (aortic arch) arteries. These become the arteries of the head and neck.
The pharyngeal pouches come from endoderm whereas the aortic arches each contain mesoderm and neural crest cells.
The left 4th pharyngeal arch gives rise to the aorta and the 3rd pharyngeal arch (right and left) gives rise to the common carotid arteries.
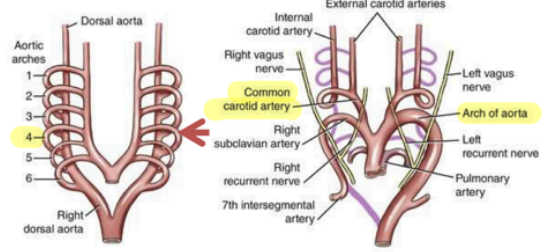
Dorsal aortic region
Arises from the 4th pharyngeal arch and gives rise to the following subregions.
Ventral vitelline vessels: Supply the GI tract.
Lateral branches: Supply kidneys and gonads
Dorsal intersegmental branches: Supply the vertebral column, body wall, and limbs
Umbilical vessels
Disappear after birth. There are two umbilical arteries. The arteries will carry deoxygenated blood away from the fetus to the placenta (to receive oxygenation).
Venous System
Vitelline region: drains blood from the yolk sac and gut tube.
Umbilical region: One umbilical vein which carries oxygenated blood (from the placenta) to the fetus.
Cardinal region: Flows into the sinus venosus and develop the venae cavae.
Arm Circulatory System
Day 27: Axial arteries develop via vasculogenesis from the somatopleuric lateral plate mesoderm.
Day 30: 7th cervical intersegmental arteries arise from the dorsal aorta and anastomose (connect) with the axial artery.
The axial artery will extend with the muscle progenitors and the ventral/dorsal muscle masses of the upper limb. Know the brachial artery of the upper arm and the interosseous artery of the lower arm.
Leg Circulatory System
Day 27: Axial arteries develop via vasculogenisis from the somatopleuric lateral plate mesoderm.
Day 30: 5th lumbar intersegmental arteries arise from the dorsal aorta and anastomose with the axial artery.
The axial artery will extend and become the external iliac arteries. From the external iliac most arteries will develop except the sciatic, popliteal, and fibular arteries.
Development of the Lymphatic System
Around 6-weeks, endothelial cells from the major veins undergo bilateral angiogenesis.
- Right and left jugular veins form (draining lymph from upper limbs, trunk, head, and neck)
- Retroperitoneal lymphatic sac forms
- Cisterna chyli forms
- Posterior lymphatic sac forms
At week 8-9, the lymphatic sacs become ducts and the cisterna chyli become the central lymph basin which drains into the thoracic duct and empties into the venous circulation.
Clinical pearls
Turner Syndrome
Blockage of lymphatics leading to cystic hygromas which often go away with age.
Milroy Disease
Inherited autosomal dominant disorder characterized by lower limb lymphedema (swelling caused by lymph accumulation). Will display as poor uptake of radioactive colloid in the lymph nodes caused by a lack of lymph vessels and abnormal function of the vessels in the legs.