Neoplasia Primer
Vocab
Neoplasia is new growth, used interchangeably with tumor.
Non-neoplastic cell proliferation is controlled cell growth induced by stimulating agent. Neoplastic cell proliferation is unregulated and autonomous cell growth which occurs and persists in the absence of inducing agent.
Metaplasia is proliferation of new types of cells, whereas dysplasia is the disorderly growth of the same cell type. Note that in dysplasia, the basement membrane remains intact.
Desmoplasia is a connective tissue response stimulated by parenchymal cells, fibrous tissue makes tumor look firm and adheres to surrounding structure.
Tumor Types
Benign
New and autonomous growth but typically confined to basement membrane which can still grow and cause problems, but does not have ability to metastasize. Usually well-circumscribed and encapsuled.
Types
- Adenoma: Glandular epithelium
- Leiomyoma: Smooth muscle
- Rhabdomyoma: Skeletal muscle
- Fibroma: Fibrous tissue
- Lipoma: Adipose tissue
Malignant
New growth that breaks through the basement membrane and has ability to metastasize. Always non-encapsulated and generally ill-defined.
Carcinomas
From epithelial tissue.
- Squamous cell: Skin, mucosal surfaces
- Adenocarcinoma: Gastrointestinal tract, liver, lung
- Small cell (neuroendocrine): Lung, prostate
Sarcomas
From mesenchymal tissue.
- Leiomyosarcoma: Soft tissues, uterus (rare)
- Rhabdomyosarcoma: Head and neck, soft tissues, Vagina
- Liposarcoma: Soft tissues, retroperitoneum
- Fibrosarcoma: Soft tissues
Lymphomas
From lymphoid tissue.
- Hodgkin Lymphoma
- Non-Hodgkin Lymphoma: B cells, T cells
Melanoma
From melanocytic cells. Derived from neural crest cells. Arises on the skin as well as several other organs. Look for asymmetric, colorful, and irregular moles.
Blastomas
From undifferentiated primitive cells. Appear as small, round, blue cell tumors in childhood.
- Neuroblastoma: Adrenal gland
- Retinoblastoma: Eye
- Lymphoma/leukemia: Bone marrow/ hematopoietic system
- Medulloblastoma: Brain/cerebellum
- Rhabdomyosarcoma: Skeletal muscle
- Wilm tumor: Kidney
- Hepatoblastoma: Liver
- Ewing sarcoma/PNET: Primitive neuroectoderm
Glioma
Central nervous system and glial cells (everywhere).
- Astrocytoma
- Glioblastoma
Differentiation
Well differentiated: Looks like normal epithelium but growing where it doesn’t belong
Moderately differentiated: Looks somewhat like the normal epithelium
Poorly differentiated: Doesn’t look like the normal epithelium at all but is still a carcinoma
Undifferentiated: Describes a tumor that cannot be distinguished based on histology
Metastasis
Characteristics
- Evading growth suppressors
- Enabling replicative immortality
- Tumor-promoting inflammation
- Activating invasion and metastasis
- Genomic instability (mutator phenotype)
- Inducing angiogenesis
- Resisting cell death
- Deregulating cellular energetics
- Sustaining proliferative signaling
- Avoiding immune destruction
Pathways
Direct extension: Invasion of surrounding tissue
Lymphatics: Lymph nodes
Bloodstream: Hematogenous
Within the body cavity: Seeding
Evaluation of Tumors
Features
Grading schema and criteria differ for every neoplasm and is assigned a low or high grade. Performed by the pathologist.
Considerations
- Differentiation
- Nuclear pleomorphism
- Tumor necrosis
- Mitotic activity
Staging
Review of tumor spread which informs prognosis. Performed by the radiologist, surgeon, and pathologist.
TNM system
- T: Tumor size/location
- N: Nodal (lymph) involvement
- M: Metastasis
Exogenous Cancer
Chemical
Examples
- Increased incidence of scrotal cancer in chimney sweepers during epidemiological studies during the Industrial Revolution
- PAH are hydrocarbons that can occur through grilling and are associated with lung/gastric cancers.
Radiation
Basal Cell Carcinoma and Squamous Cell Carcinoma are linked to cumulative exposure, while melanoma is linked to intense intermittent exposure.
Examples
- Sunlight UV B
- UV C is potent mutagen, but filtered out by ozone
- Ionizing radiation (gamma/x-ray) is associated with myeloid leukemias
Microbial
More than 15% of human cancers are known to be caused by viruses.
Important examples
- Epstein-Barr virus (HHV-4)
- Human Papillomavirus (HPV)
- Polyomavirus (Merkel cell)
Endogenous Cancer
Polyclonal cells form from many different cells, while monoclonal cells originate from single transformed cell (typically neoplastic). Every cell derived from tumor cells will be monoclonal.
Mechanisms
- Self sufficiency in growth signals (oncogenes)
- Insensitivity to growth inhibitory signals (tumor suppressor defects)
- Defects in DNA Repair
- Evasion of apoptosis
- Limitless replicative potential
- Sustained angiogenesis
- Ability to invade and metastasize
Oncogenes
Proto-oncogenes are genes necessary for cell growth stimulation. Oncogenes are a mutation of proto-oncogenes, making them hyperactive. Oncoproteins are derived from oncogenes.
RAS
RAS is a GTPase involved in signal transduction (KRA, HRAS, NRAS) and is a growth signal. Mutations in RAS can result in hyperactivation, leading to constant cell growth. RAS is mutated in 20% of all cancers.
Philadelphia chromosome
Philadelphia chromosome is when chromosome 9 and 22 swap DNA, resulting in a novel protein. This is ABL/BCR fusion protein which has high tyrosine kinase activity. Imatinib targets this drug to treat Chronic Myelogenous Leukemia (CML).
Novel fusion proteins are a great drug target as knocking it out won't affect normal cells.
Translocation of promoter regions
Increases translational activity of DNA region that promoter is moved to.
In Burkitt’s Lymphoma, the Ig gene promoter is translocated to the MYC gene, increasing MYC protein, and driving cell development.
Gene amplification
Chromosomal abnormality resulting in increased gene copies and more of the oncoprotein. HER2 is amplified in 20% of breast and ovarian carcinoma. Trastuzumab is the targeted therapy for HER2.
Tumor suppressor genes
Tumor suppressor genes are necessary for cell growth inhibition.
Two Hit Hypothesis: Two alleles must be knocked out for tumor formation (homozygous for mutated allele).
APC/B catenin
These prevent beta-catenin from entering nucleus to cause transcription. The earliest mutation in a polyp to become carcinoma in colon cancer is an APC mutation. An example of a second hit mutation could be a defect in beta-catenin to make it more active.
Retinoblastoma (RB) protein
RB protein is ubiquitous in cells and involved in cell cycle regulation. Transcriptional activation occurs only if RB is active.
Cancers are associated with a loss of heterozygosity, making the cell homozygous for the mutated allele. RB mutations occur in the E2F (transcription factor) binding pocket, making E2F constitutively active.
HPV causes RB degradation with the E7 oncoprotein.
P53
The brakes on the cell cycle. If a cell becomes stressed, P53 is upregulated and results in cell apoptosis. If P53 is mutated, the stressed cells proliferate.
P53 mutations are associated with 100% of small cell lung cancers, 80% colon cancers, 50% breast cancers. He's kind of a big deal.
HPV causes P53 degradation and telomerase induction with the E6 oncoprotein. P16 is a marker for HPV infection, suggesting P16 has been upregulated to replace P53.
Failed DNA repair
Microsatellite instability (MSI)
Microsatellites are small repeating sequences that accumulate with unfaithful replication of DNA. They are usually repaired, but in MSI, mismatch repair genes MSH2 (mut S) and MLH1 (mut L) are borked.
Colon cancer with MSI has better prognosis and is treated less aggressively.
Cancer Superpowers
Evasion of Apoptosis
Tumors can downregulate ligands, inhibit mitochondrial permeabilization, or inhibit proteins to reduce the chance of apoptosis.
Limitless replicative potential
Telomeres are end caps on chromosomes which are not fully replicated and when they're gone, the cell self-destructs to prevent cancer.
Carcinoma activates telomerase to prevent shortening.
Sustained angiogenesis
Lack of oxygen in tumor cells stimulate normal response of cells to hypoxia, increasing angiogenesis via VEGF and BFGF. They make so much there is a dysregulation of capillary growth.
Metastasis
Cadherins are downregulated in tumors, making cells less sticky. Collagenase is created by the tumor to break down junctions between cells and open the basement membrane. Benign tumors show little type IV collagenase activity.
10-20% of cancers will move to the brain, which is problematic as the brain is not readily accessible for chemotherapy.
Vocab
- In situ carcinoma: Confined to epithelium without penetration of basement membrane
- Microinvasion: Invasion through basement membrane
- Local invasion: Expansion within organ
- Local metastasis: Discontinuous spread within organ or to neighboring lymph nodes
- Distant metastasis: Spread to other organs or lymph nodes
Bony metastases
- Osteolytic lytic lesion: Tumor absorbs bone
- Osteoblastic: Tumor cells causing upregulated response in osteoblasts and resulting in more bone (common on prostate cancer)
Treatment options are mostly supportive. Bisphosphonates can reduce new bone metastases and fracture.
Paraneoplastic syndromes
Arise secondary to neoplasia. They present as symptoms associated with cancer that are not explained by tumor spread or hormones from the tumor.
Endocrinopathies
Cushing’s Syndrome
Ectopic production of Adrenocorticotropic hormone (ACTH). Found in small cell lung cancer and pancreatic neuroendocrine tumors.
Results in hypertension, muscle wasting, hypokalemia, dark skin striae.
Paraneoplastic Hypercalcemia
Release of parathyroid hormone (PTH) related peptide. Found in squamous cell carcinomas or lung breast carcinoma.
Results in lethargy, polyuria (urination), polydipsia (thirst), constipation, and abdominal pain.
Syndrome of inappropriate ADH secretion (SIADH)
Ectopic production of ADH (antidiuretic hormone). Found in small cell lung cancer.
Results in hypo-osmolar hyponatremia (too much water retention) and manifests as irritability, confusion, weakness, seizures.
Hypercoagulability
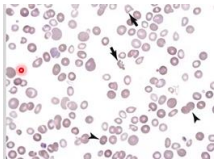
Disseminated intravascular coagulation (DIC)
Overstimulation of coagulation factors consumes factors and platelets. Found in acute leukemia, prostatic adenocarcinoma.
Results in bleeding, vascular occlusion, tissue hypoxia. Can bee identified by oddly shaped red blood cells.
Migratory thrombophlebitis (Trousseau syndrome)
Production of procoagulant factors by tumors. Found in deep seated cancers (pancreas or lung).
Results in venous thromboses in one site, with resolution, then formation in another site.
Immunologic syndromes
Paraneoplastic Myasthenia Gravis and Lambert-Eaton
Autoantibodies against Ach receptor (myasthenia gravis) or presynaptic calcium channels (Lambert-Eaton). Found in thymic carcinoma, small cell lung cancer.
Two pathways
- Antibodies against tumor cell antigens cross react with normal neuronal cell antigens
- Tumor cells' antigens mimic neural cell antigens, resulting in attack of normal cells
Results in neuromuscular symptoms, muscle fatigue/weakness.
Cancer Cachexia
Progressive loss of fat and skeletal muscle in spite of adequate nutrient intake that often happens in the end state of cancer. The tumor leads to systemic inflammation and causes wasting.