Necrosis And Apoptosis Primer
Pathology is the study of disease.
Etiology: Study of the cause of disease
Pathogenesis: Study of development of disease
Morphogenic changes: Changes in structure of tissue or organ
Clinical manifestations: Signs/symptoms of disease
Cellular Adaptation
Hypertrophy
The increase in the size of a cell and its organ. It occurs in non-mitotically active cells (e.g. muscle). It can be both natural (like the uterine wall increasing in size with pregnancy) or pathologic (enlargement of the heart from hypertension).
Etiology: Increased workload or increased stimulation
Hyperplasia
The increase in the number of cells. Can lead to increase in organ size. It occurs in mitotically active cells (e.g. epithelial). It can be both natural (lactational changes in breasts) or pathologic (benign prostatic hyperplasia).
Etiology: Increased hormonal tone or compensatory. Can be the result of growth factors, more receptors, or stem cell activation.
Atrophy
Decrease in the size of the cell and its organ. Can be both natural (especially in development) or pathologic.
Etiology: Decreased workload (disuse), denervation, low blood supply, or decreased hormonal tone. The process occurs using the lysosomal and ubiquitin/proteasome pathway to degrade cellular machinery.
Metaplasia
For more on neoplasia, see here: Neoplasia Primer.
The reprogramming of stem cells, replacing cells which are better adapted to a stressor. This generally occurs in epithelial tissues in which columnar cells become squamous cells and vice versa. This is more often pathologic and can progress to dysplasia (alteration of cell structure) and eventually cancer. For example, Barrett's esophagus can progress to adenocarcinoma of the esophagus.
Etiology: Irritation or persistent stress, such as gastric acid (Barrett's esophagus) or from tobacco smoke.
Necrosis
Tissue death. You'll see increased more red/pink staining (eosinophilia), calcification, and nuclear modifications.
Nuclear shrinkage (pyknosis) → Nuclear fragmentation (karyorrhexis) → Nuclear
dissolution (karyolysis)
Patterns
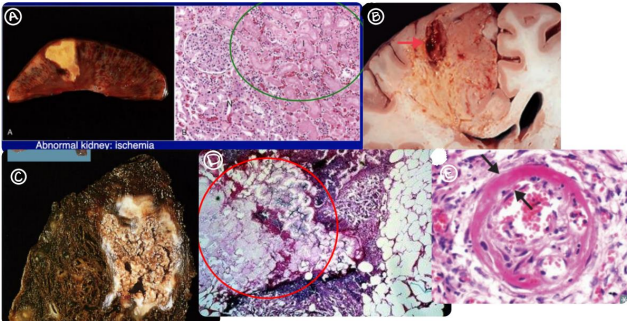
| Type | Seen In | Due To | Histology |
|---|---|---|---|
| Coagulative (A) | Ischemia/infarcts (but not in brain) | Injury denatures enzymes and blocks proteolysis | Cell shape remains, but nuclei disappear, more red/pink staining (eosinophilia) |
| Liquefactive (B) | Bacterial abscesses, brain infarcts | Neutrophils release lysosomal enzymes, digesting tissue | Cellular debris/macrophages and eventual cystic spaces or cavitation (brain) |
| Caseous (C) | Tuberculosis, fungal infection | Coagulative necrosis, granulomatous (immune) inflammation | Looks like cheese (ew), cellular debris/macrophages |
| Fat (D) | Acute pancreatitis (enzymatic) or traumatic (nonenzymatic) | Adipose tissue response to injury | Merging of adipocytes, Ca2+ salt deposition (chalky) |
| Fibrinoid (E) | Immune vascular reactions (e.g., PAN), nonimmune vascular reactions (e.g., hypertension/preeclampsia) | Accumulation of fibrin in tissue, associated with abnormal immune response | Fibrin accumulation leads to necrosis of vessel wall, stains bright pink |
Apoptosis
Caspases (cytosolic proteases) lead to cell shrinkage, chromatin condensation, membrane blebbing, and formation of apoptotic bodies. These are phagocytosed.
Intrinsic (mitochondrial) pathway
Will be triggered by loss of survival signals, DNA damage, and accumulation of misfolded proteins. Caspases will activate proteases and endonucleases to increase apoptosis.
Regulation
- BCL-2: Reduce mitochondrial pores → reduce release of Cytochrome C → reduce apoptosis
- BAX/BAK: Form membrane pores → release Cytochrome C → increase apoptosis
Inactivation of BCL-2 is part of the intrinsic pathway.
Extrinsic (death receptor) pathway
Ligand mechanism: FasL binds Fas or TNF-alpha binds TNFR
Immune cell mechanism: Cytotoxic T-cell releases perforin and granzyme B
Necrosis vs. Apoptosis
| Necrosis | Apoptosis | |
|---|---|---|
| Cell size | Enlarged | Reduced |
| Nucleus | Fragmentation, shrinkage, dissolution | Fragmentation |
| Plasma membrane | Disrupted | Altered structure |
| Cellular contents | Digested | Intact |
| Adjacent inflammation | Yes | No |
| Normal or pathologic? | Generally pathologic | Generally normal |
Cellular Accumulation
Can occur with inadequate removal via transport mechanisms, issues with degradation, or deposition of exogenous substance without the transport/degradation machinery.
- Lipid accumulations: Can be both normal and pathologic
- Protein accumulations: Can be both normal and pathologic
- Pigment accumulations: Endogenous (lipofuscin, melanin, hemosiderin or iron), exogenous (carbon, tattoos)
Calcification
Dystrophic
Results in Ca2+ deposition in diseased tissues only, causing necrosis and tumors. The serum Ca2+ levels will be normal in this case.
Metastatic
Results in Ca2+ deposition in normal tissues around the body. The serum Ca2+ levels will usual be abnormal (hypercalcemia)